Organic Brain Syndrome, a term now largely replaced in modern medical terminology, historically encompassed a range of conditions causing cognitive decline and behavioral changes due to identifiable brain damage. Understanding its historical context and the conditions it once described is crucial for appreciating the evolution of neurological diagnoses and treatments. This article delves into the causes, symptoms, diagnosis, and management of conditions that were previously categorized under this umbrella term, highlighting the complexities of brain health and the importance of accurate diagnosis.
The shift away from “Organic Brain Syndrome” reflects a move towards more precise diagnoses based on underlying causes, such as strokes, traumatic brain injuries, infections, and neurodegenerative diseases. This increased specificity allows for targeted treatment strategies and improved patient care. However, understanding the historical understanding of Organic Brain Syndrome provides valuable context for comprehending the spectrum of neurological conditions impacting cognitive function and behavior.
Organic Brain Syndrome: A Historical Overview and Modern Understanding
Organic Brain Syndrome (OBS), a term once widely used to describe cognitive impairment stemming from identifiable physical brain damage, has largely been replaced in modern medical terminology. This article delves into the history, causes, symptoms, diagnosis, and management of conditions previously categorized under the OBS umbrella, highlighting the evolution of understanding and the current approaches to care.
Definition and History of Organic Brain Syndrome
Historically, Organic Brain Syndrome encompassed a broad range of cognitive impairments resulting from demonstrable brain pathology. The term emerged in the mid-20th century, reflecting a growing understanding of the brain’s role in cognitive function. Key characteristics historically associated with OBS included memory loss, disorientation, impaired judgment, and personality changes. However, the lack of specificity and the stigmatizing nature of the term led to its eventual decline.
Modern medicine prefers more precise diagnoses that identify the underlying neurological or medical condition responsible for the cognitive impairment, such as Alzheimer’s disease, vascular dementia, or traumatic brain injury.
Causes and Risk Factors
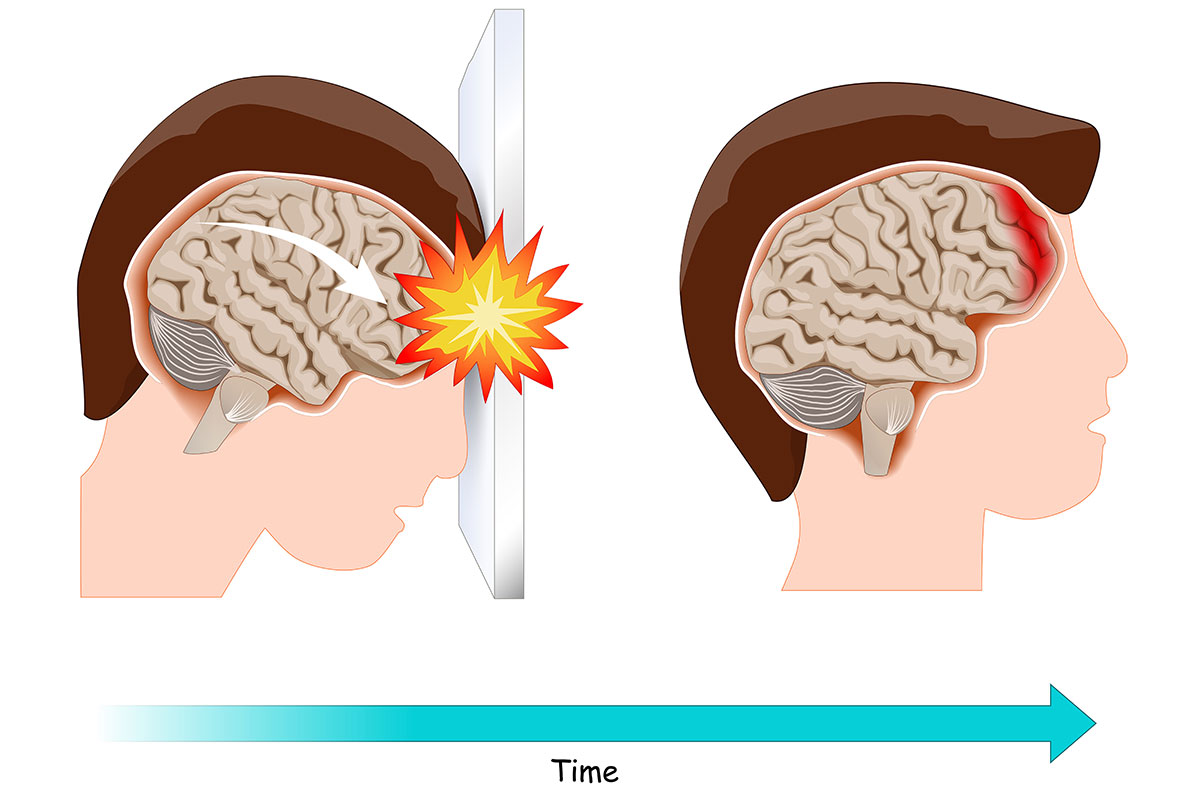
Numerous medical conditions can manifest with symptoms resembling those previously attributed to OBS. These include neurodegenerative diseases (Alzheimer’s disease, Parkinson’s disease), cerebrovascular diseases (stroke, transient ischemic attack), traumatic brain injuries, infections (encephalitis, meningitis), and substance abuse. Risk factors vary depending on the underlying cause but often include age, genetics, lifestyle choices (smoking, poor diet, lack of exercise), and pre-existing medical conditions like hypertension and diabetes.
| Age Group | Condition | Prevalence | Risk Factors |
|---|---|---|---|
| 65+ | Alzheimer’s Disease | Increasingly prevalent with age; significant portion of dementia cases | Age, family history, genetics, APOE gene variations, lifestyle factors |
| 50-70 | Stroke | Varies by region and risk factors; higher in individuals with hypertension and heart disease | Hypertension, smoking, diabetes, high cholesterol, atrial fibrillation |
| All ages | Traumatic Brain Injury | Higher in males, young adults (due to accidents), and certain professions | Falls, motor vehicle accidents, sports injuries, violence |
| Variable | Substance Abuse (Alcohol, Drugs) | Dependent on substance and patterns of use; higher in certain demographics | Genetic predisposition, social factors, peer pressure, stress, mental health conditions |
Symptoms and Manifestations
The symptoms associated with conditions previously grouped under OBS are diverse and depend heavily on the underlying cause and the extent of brain damage. These symptoms can be broadly categorized into cognitive, behavioral, and neurological domains.
Organic Brain Syndrome, a broad term encompassing various cognitive impairments, can significantly impact daily life. The stress of navigating major life changes, such as relocating, can exacerbate symptoms. For instance, someone dealing with OBS might find the process of searching for a vehicle, like browsing maui craigslist cars , particularly challenging. This highlights the need for support systems and adaptive strategies for individuals managing OBS.
- Cognitive Impairments:
- Memory loss (short-term and long-term)
- Difficulty with concentration and attention
- Impaired judgment and decision-making
- Language problems (aphasia)
- Disorientation (time, place, person)
- Difficulty with problem-solving and executive functions
- Behavioral Changes:
- Personality changes (irritability, apathy, aggression)
- Changes in mood (depression, anxiety)
- Social withdrawal
- Loss of initiative
- Neurological Symptoms:
- Motor difficulties (tremors, weakness, gait problems)
- Sensory impairments (vision, hearing, touch)
- Seizures
- Headaches
Diagnostic Procedures and Assessments

Source: amazonaws.com
Diagnosis involves a thorough assessment to identify the underlying cause of the cognitive impairment. A comprehensive medical history, neurological examination, and neuropsychological testing are crucial. Neuropsychological tests assess various cognitive domains, including memory, attention, language, and executive function. Neuroimaging techniques such as CT scans, MRI scans, and PET scans can help visualize brain structures and identify abnormalities.
Treatment Approaches and Management, Organic Brain Syndrome
Treatment strategies focus on managing symptoms and addressing the underlying cause. Medication may be used to manage specific symptoms, such as memory loss, depression, or anxiety. Non-pharmacological interventions, including cognitive rehabilitation therapy, occupational therapy, and speech therapy, aim to improve cognitive function and daily living skills. Lifestyle modifications, such as regular exercise, a healthy diet, and cognitive stimulation activities, can also play a significant role in managing the condition and improving quality of life.
Illustrative Case Studies (Hypothetical)
Source: cloudfront.net
Case 1: A 72-year-old woman presents with progressive memory loss, difficulty with language, and disorientation. Neuropsychological testing reveals significant impairments in memory and language functions. Brain imaging shows cortical atrophy consistent with Alzheimer’s disease. Treatment focuses on cholinesterase inhibitors to manage cognitive symptoms, along with supportive care and family education.
Case 2: A 60-year-old man experiences sudden onset of confusion, slurred speech, and weakness on one side of his body following a suspected stroke. Neuroimaging reveals a large infarct in the left hemisphere of the brain. Treatment includes medications to prevent further stroke, rehabilitation therapy to improve motor function and speech, and cognitive rehabilitation to address cognitive deficits.
Prognosis and Long-Term Outcomes
The prognosis and long-term outcomes for individuals with conditions previously categorized under OBS vary significantly depending on the underlying cause, the severity of the impairment, and the availability of appropriate treatment and support. Factors influencing the course of the condition include the nature and extent of brain damage, the individual’s overall health, and access to effective interventions. Early diagnosis, appropriate treatment, and supportive care can significantly improve long-term outcomes and enhance quality of life for both patients and their families.
End of Discussion
While the term “Organic Brain Syndrome” is outdated, understanding its historical significance sheds light on the evolution of neurological diagnoses and treatments. The conditions once encompassed under this term now benefit from more precise diagnoses and targeted therapies. Further research and advancements in neurology continue to refine our understanding of brain function and dysfunction, offering hope for improved prevention, diagnosis, and management of a wide range of neurological conditions impacting cognitive health and overall well-being.
Early intervention and comprehensive care remain crucial for optimizing patient outcomes.
